Immunotherapy Targeted Cancer Treatment

A Closer Look at Immunotherapy for Cancer
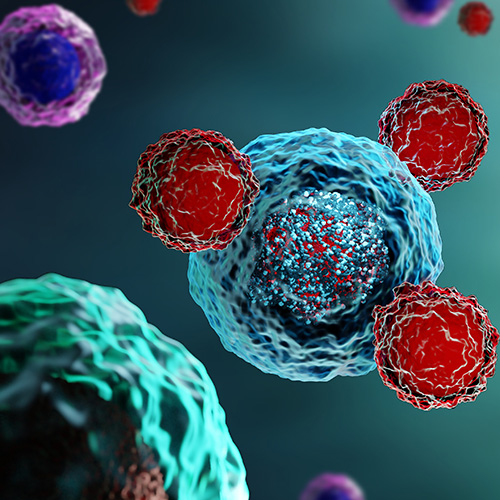
One of the most promising and successful new treatment areas for cancer is immunotherapy, which uses the body’s own immune system to find, target and fight many forms of the disease, even at advanced stages.
Immunotherapy at FCS
Florida Cancer Specialists & Research Institute (FCS) continues to make great strides in the advancements of novel therapies, including immunotherapy. Current immunotherapies available at FCS include monoclonal antibodies and checkpoint inhibitors. Typically restricted to inpatient therapy, FCS has also created a bispecific management program that allows patients to receive treatment in an outpatient setting in one of our clinics. Our physicians also partner with area hospitals to coordinate treatments offered outside of FCS.
What is immunotherapy for cancer?
Immunotherapy is one of the most promising and successful new treatments for cancer. Immunotherapy uses the body’s own immune system to find, target and fight many forms of cancer, even at advanced stages. Cancer starts when normal, healthy cells become changed or altered and begin to grow out of control. Immunotherapies boost or change the immune system to work harder and smarter to find, target and attack cancer cells. In the last few decades Immunotherapy has been approved for the treatment of many cancers, including bladder, cervical, breast, colorectal, lymphoma and melanoma, among others. Patients may receive treatments in a doctor’s office, an oncology clinic or, in some cases, in a hospital setting. Immunotherapy may be used alone or in combination with chemotherapy, radiation and/or surgery. While side effects can occur, a key difference is that they are often less severe than those encountered with conventional therapies.
Back to Top
What does immunotherapy do?
The immune system is a complex collection of organs, including the spleen, thymus and bone marrow, white blood cells, tissues and proteins. These special substances travel through the body, protecting it from viruses or germs that cause infection. When it encounters a new substance that it doesn’t recognize, it signals an alarm and works to destroy anything containing the foreign substance. Immunotherapies work to stimulate or boost the immune system’s natural defenses to work harder to fight cancer. They can be injected directly into a vein, swallowed in pill or capsule form or applied topically through a cream that is rubbed onto the skin.
Back to Top
How long does immunotherapy stay in your system?
The duration immunotherapy stays in the system varies depending on the specific type and individual response. Immunotherapy may continue to work for months or years after a patient has finished treatment. For cancer immunotherapy, effects can persist for an extended period, influenced by factors such as the type of drugs and cancer. Individual responses vary, and discussions about duration should involve healthcare professionals overseeing the specific case. They can provide personalized information based on the immunotherapy approach and medical history.
Back to Top
Who qualifies for immunotherapy?
Immunotherapy has been approved for the treatment of many cancers, including bladder, cervical, breast, colorectal, lymphoma and melanoma, among others. Patients may receive immunotherapy in a doctor’s office, an oncology clinic or, in some cases, in a hospital setting. Your oncology team can determine whether immunotherapy is a recommended option.
Back to Top
What are the signs immunotherapy is working?
Each patient is unique. Some patients have an immediate positive response while other patients respond more slowly or not at all. Immunotherapies can take longer to work than traditional treatments, such as chemotherapy or radiation. Throughout treatment, patients will have regular check-ups, blood tests or imaging scans to assess whether a tumor is responding. Researchers continue to study new and improved ways of measuring the body’s response to immunotherapy.
Back to Top
What are the types of immunotherapy?
Some of the most common types of immunotherapy used to treat cancer include:
- Bispecific antibody drug therapies bind to two specific cells at the same time. This activates the immune system to recognize and destroy certain types of cancer cells. Learn more about Bispecific Therapy at FCS.
- CarT-cell therapy is a type of cell-based treatment that involves altering immune cells called T cells (a type of white blood cell) in a laboratory so that they are better able to find and destroy cancer cells.
- Checkpoint inhibitors are drugs that block immune checkpoints, which can sometimes dampen immune system response, and allow cells to respond more strongly to cancer.
- Monoclonal antibodies are proteins that are created in a lab to act like antibodies that naturally circulate in the body. They are designed to attach themselves to single cancer cells so that they can be better seen and destroyed by the immune system.
- Vaccines boost the body’s ability to recognize and destroy or slow the growth of cancer.
What are the side effects of immunotherapy?
Immunotherapy for cancer can have side effects, and the nature and severity of these side effects can vary depending on the specific type of immunotherapy and individual patient factors. It’s important to note that not everyone will experience the same side effects, and some people may not experience any noticeable side effects. Common side effects of immunotherapy may include:
- Fatigue: Feeling tired or lethargic is a common side effect of many cancer treatments, including immunotherapy.
- Skin Reactions: Skin-related side effects such as rash, itching, or redness are common with certain immunotherapy drugs.
- Flu-Like Symptoms: Some people may experience symptoms similar to the flu, including fever, chills, muscle aches, and weakness.
- Digestive System Issues: Diarrhea, nausea, vomiting, or loss of appetite are possible side effects of immunotherapy.
- Respiratory Issues: Coughing, shortness of breath, or other respiratory symptoms may occur with certain types of immunotherapy.
- Autoimmune Reactions: In some cases, immunotherapy may cause the immune system to attack healthy cells and tissues, leading to autoimmune reactions. This can result in conditions like colitis, hepatitis, or thyroid disorders.
- Allergic Reactions: Rarely, severe allergic reactions can occur, which may manifest as difficulty breathing, swelling, or a drop in blood pressure.
More Promise on the Horizon
Every person and every cancer is unique. FCS medical oncologists work with each patient and their entire healthcare team to devise a personalized treatment plan using every resource available to achieve the best possible outcome.