Prostate Cancer 101

Men’s Health FAQ
If I had a vasecotomy can I still get prostate cancer?
Behind skin cancer, prostate cancer is the most common type of cancer for American men. In fact, the American Cancer Society estimates that 1 in 8 U.S. men will receive a diagnosis of prostate cancer. This statistic alone is enough to prompt you to start asking questions about what causes prostate cancer and whether you could be at risk.
One of the topics most often explored is the relationship between vasectomy and prostate cancer. This has been an ongoing debate in the medical community; some studies have made shaky claims that men who have had a vasectomy have an increased risk for prostate cancer. We’ve brought all perspectives here for you.
Why is there a perceived link between having a vasectomy and prostate cancer?
Many studies have concluded that there is not a direct link between vasectomy and prostate cancer. But there are still some studies, such as one conducted by the Journal of the American Medical Association (JAMA), which found a 5% increase in the risk of prostate cancer after a vasectomy. However, some of these perceived correlations at the surface level do not always indicate causation.

For example, men who have had a vasectomy tend to be more sexually active, which makes them more likely to contract a sexually transmitted infection (STI). STIs are a known risk factor for prostate cancer – as well as other types of cancer. In this case, it wouldn’t be the vasectomy that increased the risk; it would be the behavior that resulted in the STI.
Another example is the timing of your vasectomy and exams. Each year, more than 500,000 men in the U.S. choose to have a vasectomy, and most of those men get a vasectomy before age 50, which means they most likely have not begun prostate screenings. A vasectomy exam could be the first time they have had that area of their body closely inspected. This screening can lead to early detection that would not have otherwise occurred until later in life.
The good news: The American Urological Association reviewed nine major studies and concluded that men who had a vasectomy were at no greater risk of prostate cancer than men who did not have a vasectomy.
What can cause prostate cancer?
The exact cause of prostate cancer is currently unknown but under extensive research. However, studies have identified key risk factors for prostate cancer, even though we’re unsure how they might cause prostate cells to become cancer cells. Some of these risk factors include:
- Genetics – Changes in the DNA of a normal prostate cell cause 10% of prostate cancers. Certain gene mutations can pass from generation to generation. These mutations can be found in all cells in the body. As with many other types of cancer, you have a higher chance of being diagnosed with prostate cancer if a first-degree family member (e.g., father or brother) has been previously diagnosed.
- Age – The risk of prostate cancer rises as you get older. Prostate cancer is relatively rare in men younger than 40 years old, but chances of a prostate cancer diagnosis rise rapidly after age 50. About 6 in 10 cases of prostate cancer occur in men older than 65.
- Race – African American men develop prostate cancer at nearly twice the rate of White, Hispanic, or Asian men. Scientists don’t have a clear reasoning for these racial and ethnic risk differences currently, but they believe access to screenings has become a main factor in most diagnoses.
- Diet – Research has found a connection between dairy consumption and prostate cancer. Some researchers believe the strong associations between milk intake and prostate cancer could be due to milk’s fat, calcium, and hormone levels. High calcium intake, in particular, has been associated with an increased risk of advanced-stage prostate cancer.

5 warning signs of prostate cancer.
Worried that you may be at risk? While we always encourage you to speak with a medical professional directly, here are the five warning signs of prostate cancer to use as a reference. Please keep in mind that not all men show symptoms.
- Body Pain – Experiencing back pain near the spine, in the hips, or in your chest and rib area
- Urination – Having problems urinating, which includes a weak urinary stream, pain or burning while urinating, or the need to urinate more often – especially at night; in some cases, even loss of bladder or bowel control can occur
- Bleeding – Noticing blood in the urine or semen
- Erectile Dysfunction (ED) – Trouble getting an erection
- Numbness – Experiencing weakness or numbness in the legs or feet
Contact Us
Where exactly is the prostate located, and how can I get tested?
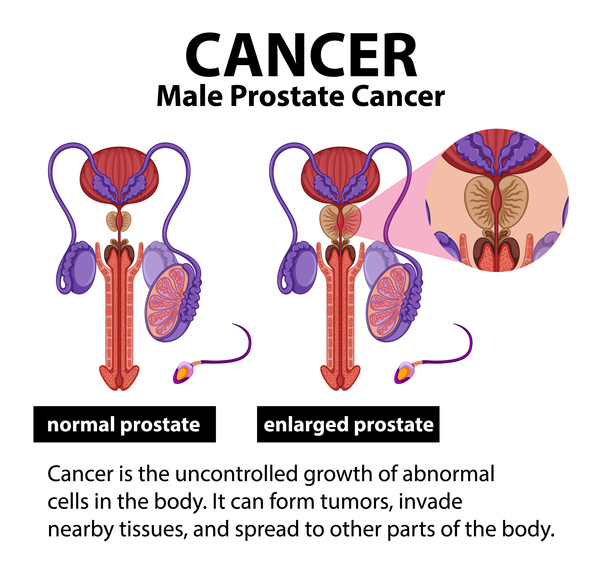
The prostate is a gland in the male reproductive system found below the bladder and in front of the rectum. Its primary function is to produce the seminal fluid that nourishes and transports sperm. There are a couple different ways to test for prostate cancer.
- Blood Test – A blood test that measures the level of prostate specific antigen (PSA), a protein made by the prostate, is often the first step in screening for prostate cancer. The higher the PSA level in the blood, the more likely that a prostate problem is present.
- Digital Rectal Exam – During a digital rectal exam, your doctor inserts a gloved, lubricated finger into the rectum to feel for any lumps or hard areas on the prostate that could indicate cancer.
If the result of either test is abnormal, your doctor may recommend a biopsy to investigate further. Current recommendations indicate that men should start screening for prostate cancer at age 50. If your physician determines you are high risk (usually due to a family history) they may want you to start screenings at age 45.
Protecting Your Prostate
While the research is unclear whether having a vasectomy directly increases the risk of prostate cancer, it’s crucial for all men – regardless of their reproductive choices – to prioritize regular prostate health checkups and screenings as they age.
Prostate cancer can affect anyone with a prostate, and early detection remains the key to successful treatment and better outcomes. So, whether you’ve had a vasectomy or not, staying vigilant about your prostate health and maintaining a healthy lifestyle are essential steps in reducing your risk and improving your overall well-being.





Comments