Endometrial Cancer - Summary, Symptoms & Treatments
Contact Us
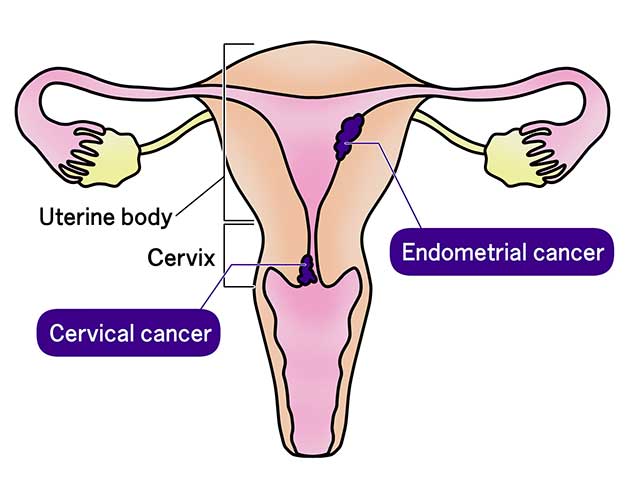
What is endometrial cancer?
Endometrial cancer is a specific type of uterine cancer. It begins in the endometrium, the inner lining of the uterus, which is the organ in a woman’s pelvis where fetal development occurs during pregnancy. Endometrial cancer is the most common gynecologic cancer and typically affects postmenopausal women.
There are two primary types of endometrial cancer:
- Type 1, known as endometrioid adenocarcinoma, is the most common type. It is often linked to excess estrogen exposure and usually grows slowly.
- Type 2, known as non-endometrioid cancers, are less common and more aggressive.
What are the signs and symptoms of endometrial cancer?
The most common signs and symptoms of endometrial cancer include:
- Abnormal vaginal bleeding, especially after menopause
- Irregular bleeding between periods or heavier than normal periods in premenopausal women
- Unusual vaginal discharge
- Watery, pink, or bloody discharge or discharge with a foul odor
- Persistent pain or pressure in the lower abdomen or pelvic area
- Pain during intercourse
- Unexplained weight loss
- Feeling a frequent urge to urinate or pain while urinating.
If you experience any of these symptoms—especially postmenopausal bleeding—it is important to see a doctor for further evaluation. Early detection greatly improves the chances of successful treatment.
How is endometrial cancer diagnosed?
Diagnosing endometrial cancer begins with a physical exam so that your doctor can evaluate the symptoms you are experiencing and discuss your health history in detail. A pelvic exam can help check for abnormalities in the uterus and surrounding organs. Diagnosis may also include a combination of imaging tests, including ultrasound. In some cases, a biopsy may be performed to obtain a tissue sample for examination under a microscope. If a biopsy is inconclusive or more tissue is needed, a D&C (Dilation and Curettage) may be recommended. During this procedure, the cervix is dilated and a larger sample of the uterine lining is scraped for examination.
Back to Top
What causes endometrial cancer?
Endometrial cancer is primarily caused by genetic mutations in the cells of the endometrium (the inner lining of the uterus). These mutations cause cells to grow uncontrollably, forming a tumor. While the exact cause of these mutations is not always known, several risk factors contribute to their development.
Factors that may increase risk of endometrial cancer include:
- Hormonal imbalance: high levels of estrogen without enough progesterone can overstimulate the endometrial lining, leading to abnormal cell growth.
- Age: endometrial cancer occurs most often in women over age 50, particularly after menopause.
- Menstrual history: early onset of menstruation (before age 12), late menopause (after age 55) or never having been pregnant
- Obesity: fat tissue converts androgens into estrogen, increasing cancer risk. Obese women have a two to four times higher risk of endometrial cancer.
- Sedentary lifestyle: lack of exercise contributes to obesity and hormonal changes.
- Diabetes and insulin resistance
- Certain genetic conditions or a family history of uterine or colon cancer.
- Use of tamoxifen, a drug used to treat breast cancer or prior radiation therapy to the pelvis.
Is endometrial cancer genetic?
Endometrial cancer can be genetic, but most cases occur due to acquired mutations rather than inherited ones. The most well-known genetic link to uterine cancer is Lynch syndrome, a hereditary condition that increases the risk for certain cancers. It is best to talk with your doctor about any genetic factors that may be present.
Back to Top
Is endometrial cancer curable?
The success of treatment for endometrial cancer depends on several factors, including the type, stage and grade of the cancer at diagnosis, and the treatment options available. Some types are highly treatable, especially when caught early, while others can be more challenging to cure.
Back to Top
Is there a screening test for endometrial cancer?
Currently, there is no standard screening test for endometrial cancer. However, certain tests and evaluations are used for women who have symptoms or are at higher risk. It’s important for women to be aware of symptoms and risk factors and to consult a doctor if they experience unusual changes. Regular gynecological exams are important for early detection and diagnosis.
Back to Top
What are the best things women can do to reduce the risk of endometrial cancer?
While there is no guaranteed way to prevent endometrial cancer, women can consider the following strategies to lower their risk:
- Maintain a healthy weight with a balanced diet and regular physical activity.
- Limit alcohol intake.
- Limit use of Hormone Replacement Therapy (HRT), which has been linked to an increased risk of ovarian cancer. Women should discuss risks and benefits with their healthcare provider.
How is endometrial cancer treated?
Each patient and each cancer is unique. Treatment options for endometrial cancer depend on a number of factors, including the specific type, size, location and grade of the tumor and the patient’s overall health Surgical removal of the uterus, a hysterectomy, is the most common treatment. Treatment options can also include radiation therapy, hormone therapy, chemotherapy or immunotherapy. At FCS, physicians develop a personalized treatment plan in partnership with patients. FCS is committed to advancing treatment and outcomes for patients with gynecologic cancers. Each year, dozens of clinical trials are conducted within FCS to find newer, better and more targeted treatments for the different types of gynecologic cancer.
Back to Top